The Winter Plan for Mental Health – Where are We Now?
Mental Health has been significantly impacted as a result of the pandemic. Some unintended consequences of the public health measures, which kept us safe from infection, were a severing of social contact and support, whilst many experienced trauma and grief.
Those drawing on care and support tell us that their mental health has deteriorated during the pandemic; we know, for example, that social care staff are five times more likely to have reported serious mental health challenges in the last year.
The Mental Health and Wellbeing Policy and Oversight group (POAG) brings together people with lived experience, voluntary and community providers of mental health social care, ADASS and key partners such as NHSE and the LGA. In July 2021, the group developed and submitted recommendations to the DHSC on what a winter plan for mental health should look like. This was against a background of concerns that previous plans had focused mostly on physical health and hospital discharge, and that the first Covid-19 adult social care winter plan had centred chiefly on supporting care homes.
The group chairs, Melanie Brooks (Corporate Director for Adult Social Care for Nottinghamshire and ADASS MH Network Policy Lead) and Kathy Roberts (CEO of the Association of Mental Health Providers), reflect on what has been achieved since the government published the winter plan and the impact that the July 2021 report has had on the policy environment.
Every day, Kathy and Melanie see the essential value of social care – people at the point of real need, directly accessing care and support, and benefitting from the input of the social care sector into their future choices, their sense of control and their capability for independent living.
There have been gains in the recognition, nationally, of the role of social care. For example, across the breadth of mental health services provided to our citizens, there is a greater alignment with social care contained in the government’s healthcare winter plan. Furthermore, Adult Social Care now has a plan in its own right, which references the broader needs of people within their communities.
However, since the mental health recommendations were published, two core areas of focus have risen to the top of the agenda, and there is much work to do to ensure that these are reflected in national planning for both health and social care.
The first of these areas is the maintaining of a strong and resilient workforce, able to provide continuity of care, and which is recognised as being the of highest priority in order to maintain safe services. Recruitment and retention may be felt most acutely in certain social care services, but it is also a growing concern within mental health social care.
Second is the need for strategic and transparent funding across our integrated commissioning pathways, to promote good mental health and crisis support.
Without prioritising of investment, in both workforce and care and support services, the result will be poor mental health care. Melanie and Kathy share with us their concerns, that these effects are already being felt within health and social care acute services.
- Melanie
“Good mental health starts and ends with people and their networks, and is supported by connected communities & systems, which focus as much on social support as they do on medical treatment.” - Kathy
“There is huge and untapped potential within social care, for the transformation of mental health services.
“A major obstacle for the development of the social care workforce in transformation planning is the partial understanding of its contribution to mental health. This has to form a key starting point for building a new culture of effective workforce support.”
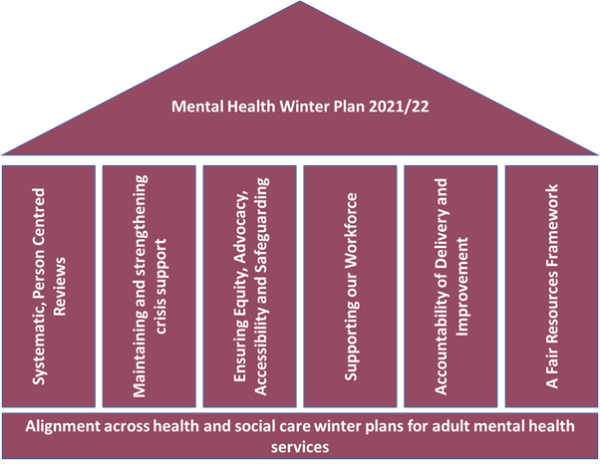
The POAG report focuses on the following principles, for surviving resurgent covid infections and ensuring the wellbeing both of staff and of those using services:
- Approaches to mental health should be coproduced with those who have experience of the current system, and need to be resourced and supported across the national and local government systems, the NHS and the voluntary, community and social enterprise sector (VCSE).
- Social Care must be an equal partner with the NHS at all levels within the system, and the winter plan for the sector must align with the NHSEi plans for adult mental health services in 2022/23 and beyond.
- The winter plan and in fact all strategic mental health planning should focus on the following critical pathways;
- Melanie
“What we have been challenged by over the last few months is the fundamental lack of capacity to implement the recommendations fully across the country.
“Many councils will have quickly established local plans over winter to ensure that access to support in a crisis remains at the forefront of their responsive, person-centred mental health services.”
Maintaining and strengthening Crisis Support ensures that there is a local alternative to A&E for people in crisis, such as via VCSE crisis services.
The Integrated Care System (ICS) confirmed, in writing, their local arrangements for people in acute mental distress, in line with their legal responsibilities under s140 of the Mental Health Act (confirming where to take an adult or child who is in acute mental distress, and who cannot wait for other interventions).
- Kathy
“The overwhelming message from people with lived experience of severe and enduring mental health needs is the importance of continuity of care through the pandemic.
“It is worth considering taking contact appointments into the community, and to the people being supported, rather than always expecting the service user to come to the provider.”
Systematic and person-centred reviews must consider whether:
- arrangements are in place for all those known to mental health services, to meet with their key workers regularly and to have updated their crisis plans
- commissioned services have a plan in place which evidences how they are keeping in touch with services users (offering remote and face to face contact).
Ensuring Equity, Advocacy, Accessibility and Safeguarding:
Crisis and other support services should be open and accessible to all, including with those who are homeless or have no recourse to public funds, and with those from communities at greater risk of formal admission (such as migrants and those from non-white British backgrounds).
We also recommend reviewing the local arrangements in place to support the ‘Breathing Space’ mental health debt management scheme, ensuring that these are publicised and resourced by Association services in partnership with Mental Health Provider Trusts.
- Kathy
“Our members’ reach is vast, meeting the needs between them of what we believe to be over eight million people with mental health needs in England and Wales. Crucially, this social care and support allows people with mental health needs to build resilience and autonomy in their lives.” - Melanie
“As we move into new systems of accountability and assurance under the CQC, local authorities and their partners need to understand more, and in greater detail, what is happening in their communities.”
“As we move into new systems of accountability and assurance under the CQC, local authorities and their partners need to understand more, and in greater detail, what is happening in their communities.”
To ensure transparent and fair resourcing plus accountability, now is the time when we must communicate effectively, build workforce capacity over the longer term, and make sure that mental health knowledge and skills are spread across the adult and child social care services;
- Adult mental health service performance data must be collected, such as; trends in urgent and emergency mental health act assessments both in number and location (police stations, A&E, places of safety); delays in admissions from community settings, as well as after emergency assessments, and the reasons (e.g. lack of police/AMHPs/s12 doctors/beds); out of area placements; S140 usage.
The ICS/Health and Wellbeing Board should routinely see data that provides assurance on delivery and improvement including, for example:
- Are personal health and care budgets, and direct payments, available and used by those with s117 entitlements?
- Is the Better Care Fund being used effectively to invest in community mental health support, in particular in social support to avoid crisis, reablement and recovery services, including supported housing as well as supporting carers, and increasing access to advocacy?
In conclusion, Melanie and Kathy both highlight the importance of working together across systems, to service seasonal pressures and to transform and improve the mental health of our nation, and they do both welcome some of the vision in the recent White Paper, offering strong policy thinking.
- Kathy
“We can see that the paper talks about the crucial elements for good care and support that the Association has long advocated for – choice, control, quality, accessibility. Now we must ensure that there is enough funding to meet the rising costs and demands for mental health social care.”